Burns and Scalds
Types of burn:
There are 3 main categories of burn:
- Superficial: Characterised by redness, tenderness and swelling. Only the very surface of the skin is affected. Sunburn is a good example.
- Partial thickness: Characterised by redness, pain and blistering. The epidermis (top layer of skin) is completely destroyed. Large areas of partial thickness burns need medical attention.
- Full thickness: The burn is deep through the layers of skin, which may be charred, waxy or pale. Usually not that painful due to nerve damage. Need urgent medical treatment.
- Full thickness burns (all the way through the skin to the underlying tissue).
- Burns to the face, hands, feet or genital area.
- Burns which extent the entire way around and arm or leg.
- Partial thickness burns larger than 1% of the casualty's body surface area (about the area covered by the palm of the casualty's hand).
- Superficial burns larger than 5% of the casualty's body surface area (about the area covered by 5 palms).
- Burns with a mixed pattern of varying depths.
- Any burn you are unsure of - better safe than sorry.
- Cool the burn area with cold liquid for at least 10 minutes.
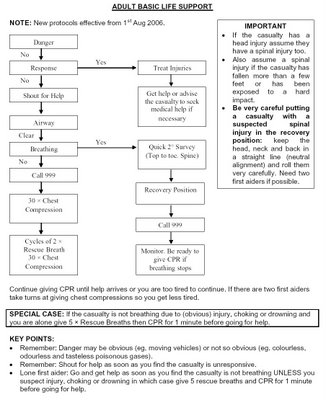
- Severe burns: Lay the casualty down. Call for an ambulance. Be prepared to give CPR if the casualty stops breathing.
- Keep cooling the burn until the pain subsides.
- Put on disposable gloves if available. Gently remove any rings, watches, belts or clothing before the tissues begin to sell. Do not remove clothing stuck to the wound. Do not put any ointments or lotions on the wound.
- Cover the wound with a clean non-absorbent dressing - clingfilm is ideal.
- Monitor the casualty until help arrives. Treat for shock if necessary.