Recognition:
Choking is caused by a foreign object becoming lodged in the top of the airway. Choking comes in two categories - mild and severe. In all cases the casualty will be in visible distress, trying to gasp for breath and will become discoloured in the face. A casualty with mild choking will be able to cough out the obstruction by themself. In the case of severe choking the casualty will struggle to cough, speak and breathe - they need urgent help to remove the obstruction before they lapse into unconsciousness.
Treatment (Adult or Child):
If the casualty appears to be choking:
- Ask the casualty to cough. If the obstruction becomes dislodged remove it from the casualty's mouth.
- If the obstruction remains give the casualty up to 5 sharp back blows:
- Strike between the shoulder blades in a firm upwards motion.
- If the obstruction becomes dislodged remove it from the casualty's mouth, if not perform abdominal thrusts.
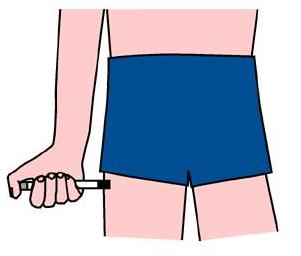
- If the obstruction remains give the casualty up to 5 abdominal thrusts (picture above):
- Put your arms around the casualty from their back to front.
- Position your hands over the stomach of the casualty.
- Make a fist with one hand and grasp the fist with the other hand.
- Firmly pull your fist in an inwards and upwards motion.
- If the obstruction becomes dislodged remove it from the casualty's mouth.
- Give two more cycles of back blows and abdominal thrusts if the obstruction is still not clear.
- If the obstruction is not clear after your 3 cycles of back blows and abdominal thrusts call 999.
- Continue until help arrives.
Treatment (Infant <1 year)
If the child is visibly distressed, unable to cough or breathe:
- Lay the infant along your forearm with their head low and support their back and head.
- Give up to 5 back blows:
- Be firm but not too hard.
- If the obstruction becomes dislodged remove it from the casualty's mouth.
- If the obstruction remains turn the casualty on to their back and give up to 5 chest thrusts:
- Use two fingers, push inwards and upwards (towards the head) against the infants breastbone, one finger's breadth below the nipple line.
- The aim is to relieve the obstruction with each chest thrust rather than necessarily doing all five.
- Give two more cycles of back blows and chest thrusts if the obstruction is still not clear.
- If the obstruction is not clear after your 3 cycles of back blows and abdominal thrusts call 999.
- Continue until help arrives.